LANCET COUNTDOWN ON HEALTH AND CLIMATE CHANGE
POLICY BRIEF FOR THE UNITED STATES OF AMERICA
DECEMBER 2020
The state of climate change and health in the United States
In the United States (U.S.), the human suffering and death during the COVID-19 pandemic demonstrate the harsh consequences that can occur when science is disregarded and responses to existing evidence are delayed, ineffective, and inequitable – or altogether absent. Importantly, the toll of the pandemic should be seen as a forewarning of the future; there will be far-reaching and accelerated health consequences of climate change if the U.S. fails to appropriately respond to the current evidence. Globally, greenhouse gas (GHG) emissions must be reduced by almost half over the next decade to keep global temperature rise to “well below 2°C”, requiring a 7.6% reduction in GHG emissions every year._1
The U.S. also faces a long-overdue reckoning for centuries of systemic racism, which continues to drive many health inequities and injustices._2 Climate change exacerbates the health consequences of both the COVID-19 pandemic and systemic racism (see Appendix Compounding Crises Case Study), especially against the backdrop of a neglected public health system. Climate change action, perhaps now more than ever, is a critical component for achieving optimal health and health equity in the U.S.
The effects of climate change worldwide and in the U.S. are undeniable and worsening, with wide-ranging impacts on health and the economy._3 Globally, the six warmest years in recorded history occurred between 2014-2019, with 2019 the second warmest._4 In the U.S., states like Alaska, Georgia, and North Carolina had record high temperatures in 2019._5
In 2019, older persons, or individuals over the age of 65, experienced over 102 million* F1 more days of heatwave exposure in the U.S. compared with the 1986-2005 baseline._3 Eight out of the ten highest ranking years of heatwave exposure among older adults, a population especially vulnerable to heat, have occurred since 2010 in the U.S._3In the past two decades, heat-related mortality F2 for older persons has almost doubled, reaching a record high 19,000 deaths in 2018._3
The U.S. saw a total of 2 billion* potential hours of labor lost due to extreme heat across the service, manufacturing, agricultural, and construction sectors in 2019F3 (with 540 million* potential hours lost in construction alone), placing the 2015-2019 average 63%* higher than the 1990-1994 average._3 A conservative estimated total of $45 billion dollars* of potential earnings were lostF4 across these four sectors in 2015._3
Climate change alters rainfall patterns and intensifies extreme weather events. In 2019, the U.S. had its second wettest year on record with many Midwestern and Central states logging unprecedented levels of rainfall._5 Fourteen weather and climate disasters in 2019 each caused damage of at least one billion dollars, not including health-related costs, and most of these events struck the Central states. Three flooding events along the Missouri, Mississippi, and Arkansas Rivers totaled over $20 billion in damages (see Appendix 2019 Floods Case Study). These disasters had widespread health effects and may have exacerbated food insecurity (see Appendix Promoting Food Security Case Study).
Climate change, through drier weather and higher temperatures, can also increase the likelihood of wildfire events, as has been repeatedly exhibited in Western states. Individuals in the U.S. experienced 1.85 billion* more person-days (one person experiencing one day) of exposure to high wildfire risk in 2016-2019 compared to 2001-2004, which is a 19%* increase._3 Wildfires generate dangerous particulate air pollution, with local and long-range health impacts (see 2018 and 2019 Briefs), and have contributed to a decline in U.S. air quality since 2016._6
While extreme weather events garner media attention, climate change has ripple effects on health in the U.S. that are often less obvious, such as worsening pollen levels, mental health, water-borne diseases (e.g., Vibrio), and human migration and displacement._7 As the health harms and urgency grow, U.S. health professionals and researchers are engaging at the intersection of climate change and health like never before, as exemplified by a nearly eight-fold increase*F5 in research publications on climate change and health between 2007 and 2019._3
This fourth annual U.S. Policy Brief, supported by 70 institutions, organizations, and centers, uses data from the 2020 global Lancet Countdown report and supplemental sources to highlight the opportunities in the U.S. to respond to these threats. No one is immune to these health risks. While time is running out, there is still an opportunity for decisive action to lessen the severity of climate change impacts by prioritizing a healthy future for all._8
Critical Insight:
Vibrio are a type of bacteria found in coastal waters that can cause water- or food-borne disease. The suitability of coastal waters for growth of these bacteria has increased. In the Northeast, it has increased by as much as 99%* over the past five years._3 Warmer waters with optimum salinity in estuaries, driven by climate change-related warming water temperatures, sea level rise, heavy rainfall, and nutrient changes, are associated with increased concentrations of Vibrio._9, _10, _11, _12
Models of the Chesapeake Bay predict expanded habitats and higher summertime concentrations of V. vulnificus and V. parahaemolyticus._10 One simulation suggests that by 2100, waters along U.S. coasts may provide a suitable habitat for V. cholerae, which causes cholera and is currently almost nonexistent domestically._13 Flooding fueled by climate change is also of concern; along the Gulf Coast, cases of non-cholera Vibrio illnesses increased after Hurricane Katrina._14, _15, _16
Implications for health
People can become infected with waterborne Vibrio bacteria (V. vulnificus, V. parahaemolyticus, and V. cholerae) when an open wound is exposed to contaminated saltwater, or by eating contaminated seafood._17 Vibrio can cause severe diarrhea, wound infections, and blood infections that can be life-threatening._17, _18
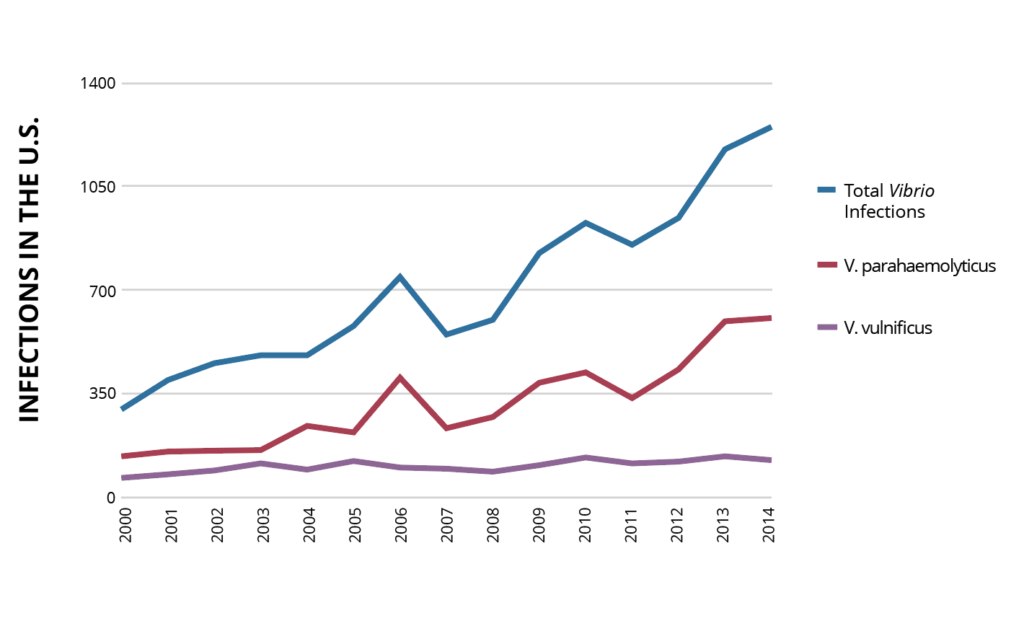
Reported Vibrio infections in the U.S. are increasing (Figure 1)_17 and expanding to new geographic regions._19, _20 The death rate is 20% for flesh-eating skin infections and exceeds 50% when infection spreads throughout the body; infections are becoming harder to treat given the bacteria’s rising resistance to antibiotics._21, _22 Individuals with diabetes, liver disease, and compromised immune systems are at greatest risk for serious complications including limb amputation and organ failure._17
Figure 1: Total reported infections of non-cholera Vibrio species in the U.S., 2000-2014.
Data from U.S. Centers for Disease Control._17 Vibrio infections became a reportable disease in 2007.
A path forward
To address the health harms from Vibrio, public health organizations and policymakers should prioritize aggressive climate change mitigation efforts. These efforts can reduce warming of water, sea level rise, and flooding, all of which increase suitability for Vibrio bacteria. To reduce the risk of Vibrio infections, public health protocols and public education should incorporate seasonality and updated location-specific hazards. The National Shellfish Sanitation Program has risk management plans for shellfish sold to eat,_23 and Maine implemented “time temperature” regulations to reduce the time for bacteria to multiply, thus limiting the potential for infection._24 In addition, California saved lives by restricting the sale of untreated raw oysters from the Gulf Coast from April to October._25 Opportunities abound to expand public health messaging in restaurants and healthcare settings to better target high-risk populations._26, _27, _28
RECOMMENDATIONS
The U.S. should rapidly and urgently implement the following recommendations in an equitable and just fashion so that every person can live with dignity and in good health.
 Transition to healthy, sustainable agricultural practices: Implement agriculture policies and invest in programs that can foster improved health from a reduction in particulate air pollution and GHG emissions, such as reducing the need for nitrogen fertilizers.
Transition to healthy, sustainable agricultural practices: Implement agriculture policies and invest in programs that can foster improved health from a reduction in particulate air pollution and GHG emissions, such as reducing the need for nitrogen fertilizers.
 Remove U.S. fossil fuel subsidies: Eliminate fossil fuel subsidies and reduce investments in new fossil fuel exploration and production.
Remove U.S. fossil fuel subsidies: Eliminate fossil fuel subsidies and reduce investments in new fossil fuel exploration and production.
 Shift to zero-carbon electricity: Urgently transition to zero-carbon electricity generation by 2035 that is affordable for all.
Shift to zero-carbon electricity: Urgently transition to zero-carbon electricity generation by 2035 that is affordable for all.
 Increase access to healthy transport options: Rapidly invest in enhanced active transport infrastructure and affordable, accessible zero-carbon public transportation, electric vehicles, and charging stations.
Increase access to healthy transport options: Rapidly invest in enhanced active transport infrastructure and affordable, accessible zero-carbon public transportation, electric vehicles, and charging stations.
 Strengthen the public health system: Increase and sustain investments in public health to protect against the accelerating health threats of climate change.
Strengthen the public health system: Increase and sustain investments in public health to protect against the accelerating health threats of climate change.
 Invest in a healthy recovery from the COVID-19 pandemic: Implement a ‘quadruple benefit’ COVID-19 recovery plan that works toward a stable climate, protects public health, promotes a sustainable economy, and creates an equitable society.
Invest in a healthy recovery from the COVID-19 pandemic: Implement a ‘quadruple benefit’ COVID-19 recovery plan that works toward a stable climate, protects public health, promotes a sustainable economy, and creates an equitable society.
Climate change exacerbates health inequities and injustices
Climate change disproportionately harms those with the fewest resources and the least capacity to respond to threats, as explored in the 2019 Brief._29 These harms are further compounded by the impacts of both historic and current discriminatory practices that cause today’s racial health inequities. For example, although redlining, a racist housing practice that targeted Black people, was outlawed in 1965, Black Americans in previously redlined areas continue to have higher rates of asthma and preterm births today._30,_31
These patterns of inequity have been made more apparent during the COVID-19 pandemic, with rates of infections in Black, Latino, and American Indian/Alaskan Native people more than 2.5 times that in White, non-Latinx people._32 Even today, urban redlined areas are almost universally hotter than neighboring areas,_33 due to factors like lack of tree cover (see Appendix Urban Green Space Case Study), and closer proximity to large roadways and industry – which increases exposure to air pollution._34
Agricultural interventions that address climate change offer broad health benefits
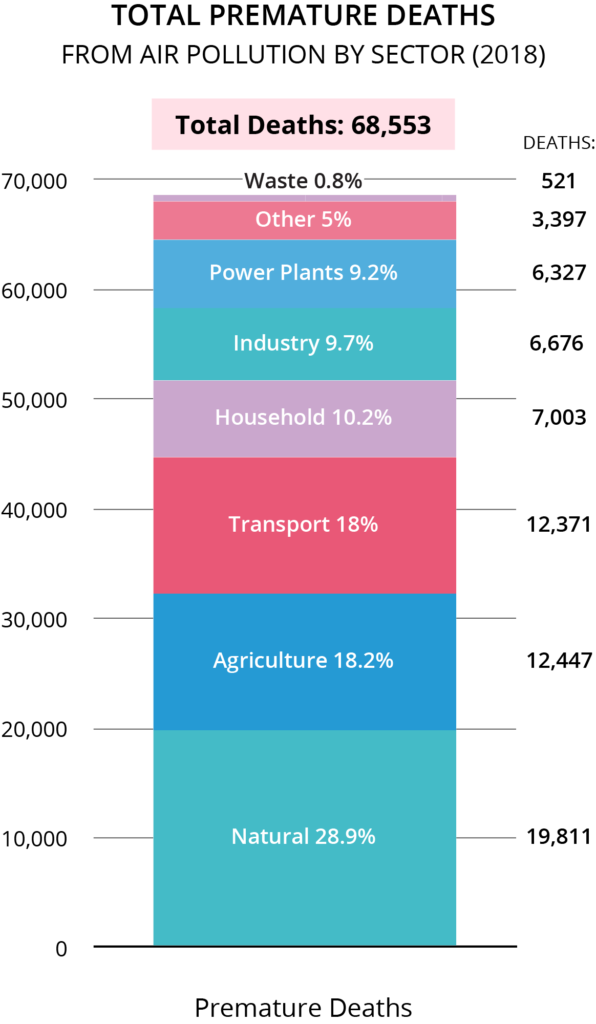
While often less recognized, U.S. agricultural practices are a leading contributor to particulate air pollution and GHG emissions, making agriculture an important mechanism to improve health and act on climate change. The agriculture sector contributed to more than 12,000 premature deaths* in the U.S. in 2018 from the tiny, health-harming air pollution particles known as particulate matter 2.5 microns in size, or PM2.5 (see Figure 2). The primary source of agricultural air pollution is ammonia, which combines with pollutants from combustive sources, such as vehicles and power plants, to create PM2.5.
This ammonia arises largely from livestock, their manure, and the application of synthetic nitrogen fertilizer to cropland. In addition, agricultural production and the associated deforestation to create land for crops and livestock accounted for almost 12.5%F6 of all U.S. GHG emissions in 2018._35 The agricultural sector is also the leading source of two major GHGs, methane (CH4) and nitrous oxide (N2O), which are nearly 85 to 265 timesF7 more potent than carbon dioxide (CO2), respectively.
Ultimately, supporting healthier and more climate-resilient U.S. agriculture that reduces air pollution and GHG emissions requires a systemic approach from production to consumption, along with recognition that agriculture is a climate change solution. Interventions such as planting cover crops can help farmers reduce the need for nitrogen fertilizers, improve soil health, diversify production systems, and increase soil resilience to droughts and floods._36 Examples of initiatives that contribute to achieving desired goals include the U.S. Department of Agriculture’s Conservation Stewardship Program and Whole Farm Revenue Protection initiative, and bipartisan bills like the Cover Crop Flexibility Act.
Figure 2: Premature deaths from ambient PM2.5 air pollution by sector in the U.S. in 2018._3
Note: Natural particulate air pollution includes natural sources like sand or sea salt.
Critical Insight:
This section provides further detail on how climate change action in the agriculture sector can also benefit health through a reduction in air pollution. Agriculture itself is impacted by climate change as, for example, crop yields decrease,_37, _38, _39 and agriculture is an important target for climate action.
Agriculture contributes 12.5%F8 of U.S. greenhouse gas (GHG) emissions with about 50% arising from soil management practices (e.g., application of synthetic nitrogen fertilizers) and 35% from livestock enteric fermentation (e.g., cow belching) and manure management._40 In addition, three-fourths of human-caused nitrous oxide (NOx) emissions arise from agricultural soils, and livestock production is the largest source of methane (CH4) emissions in the U.S. – both potent GHG emissions ,as noted in the U.S. Policy Brief._40
Overall agricultural GHG emissions increased around 11% between 1990 and 2018, outpacing the overall rise in U.S. GHG emissions of only 3.7%. Nitrous oxide and methane emissions related to manure management increased nearly 60% with the rapid rise in concentrated livestock production._40 These sources are also intricately connected with the generation of ammonia, which reacts in the atmosphere to form fine particulate matter (PM2.5), one of the most harmful forms of air pollution.
Agricultural climate change action can reduce air pollution and benefit health
The agricultural sector has been estimated to be responsible for close to 20% of all human-caused air pollution in the U.S._41 Over half of the ammonia, the primary source of agricultural air pollution as outlined in the U.S. Policy Brief, comes from livestock and their manure, while nearly a third comes from synthetic nitrogen fertilizer on cropland._42
A study found that the Midwest “corn belt” contributed to approximately 4,300 premature deaths annually from the particulate matter air pollution related to corn production, further demonstrating the significant health impacts._43 The average estimated damages associated with these deaths is $39 billion per year, which often exceeds the market value of the corn. Ammonia emissions from synthetic nitrogen fertilizers and manure drove more than 70% of these deaths.
In addition, higher ammonia concentrations in the air are associated with reduced lung function in adults and asthma in children who live near Concentrated Animal Feeding Operations (CAFOs)._44,_45 This is yet another avenue of health harms for already vulnerable agricultural workers (see 2019 Appendix), who are largely Latino and have higher rates of respiratory symptoms._46, _47
The health effects of agricultural pollution are not limited to agricultural areas, as pollutants can travel hundreds of miles from their source._45,_48 Moreover, nitrates from agriculture sources have implications for illness beyond just air pollution, such as the health harms (e.g., cancer, thyroid disease, and fetal defects) associated with the ingestion of nitrate contaminated water._49
Placing health as a driver for climate change action in agriculture
The complex U.S. agricultural system has a variety of stakeholders, which means there is a wealth of opportunity for action across both consumption and production that will have sweeping benefits for climate change and health. Alterations in consumption include a shift toward plant-based diets, reduced average consumption of meat, and reduced food waste._50 More generally for production, this should include a shift away from current large-scale industrial agricultural practices to models like regenerative agriculture._50 Broadly, regenerative agriculture consists of practices that rehabilitate and restore degraded farmland, benefiting the farmer and crops and combating climate change.
More specifically, in addition to working on GHG emission reduction, on-farm interventions can target fertilizer and manure management as a way to reduce ammonia-related air pollution. A crucial intervention is using appropriate fertilizer and manure sources at the right rate, time, and place, and incorporating or injecting manure into cropland soil to avoid ammonia losses to the air._51,_52 Other beneficial practices include low-protein feed additives, use of cover crops, improved manure storage, methane capture, and strategic use of natural infrastructure.
Research shows that improved nutrient management on cropland could reduce nitrous oxide emissions by 33%,_53 and covering manure storage on confined dairy and swine operations could reduce overall manure methane emissions by 50%._54 Policies and programs that encourage safe nitrogen balances or enable markets for biomethane are a part of this solution.
There are also broader food system reforms at the industrial level that can be implemented to curb rapid expansion of livestock production and the resulting food system emissions, such as those from the production of livestock feed crops. Both the American Public Health Association and the National Association of County and City Health Officials call for a moratorium on all new and expanding Concentrated Animal Feeding Operations until adequate public health protections are in place._55 Many of these suggested approaches also enhance carbon uptake by soil, make farms more resilient to climate change-related floods and droughts, and benefit human and livestock health._56,_57
Fossil fuels drive air pollution and climate change while U.S. subsidies effectively finance the adverse health consequences
The production and use of fossil fuels — coal, oil, and natural gas — generate air pollution that harms health and GHGs that drive climate change (Figure 2). A just and equitable transition away from fossil fuels that minimizes the health harms of climate change would also improve health and save lives immediately by reducing air pollution and providing other health benefits. However, current U.S. fossil fuel subsidies increase and lock in fossil fuel dependence, and in effect finance the adverse health consequences of fossil fuel production and use: illness, death, health care disruptions, and intensifying climate change impacts. In a 2015 self-review, the U.S. government identified 16 fossil fuel subsidies in the form of federal tax expenditures that amounted to $4 billion per year,_58 and it committed to removing them by 2025._59
Estimates vary widely depending on definitions, but current estimates of subsidies for extraction and production of fossil fuels total at least $20 billion per year._60 Subsidies amplify profits for the fossil fuel industry and allow more extraction to occur than would otherwise be economically viable in the U.S._61,_62 Furthermore, the continued expansion of fossil fuel production is inconsistent with the international Paris Agreement’s goal of keeping global warming to well below 2°C and pursuing efforts to limit warming to 1.5°C._63
Figure 3: The relationship between air pollution and climate change and the near-term health benefits of climate action._64,_65
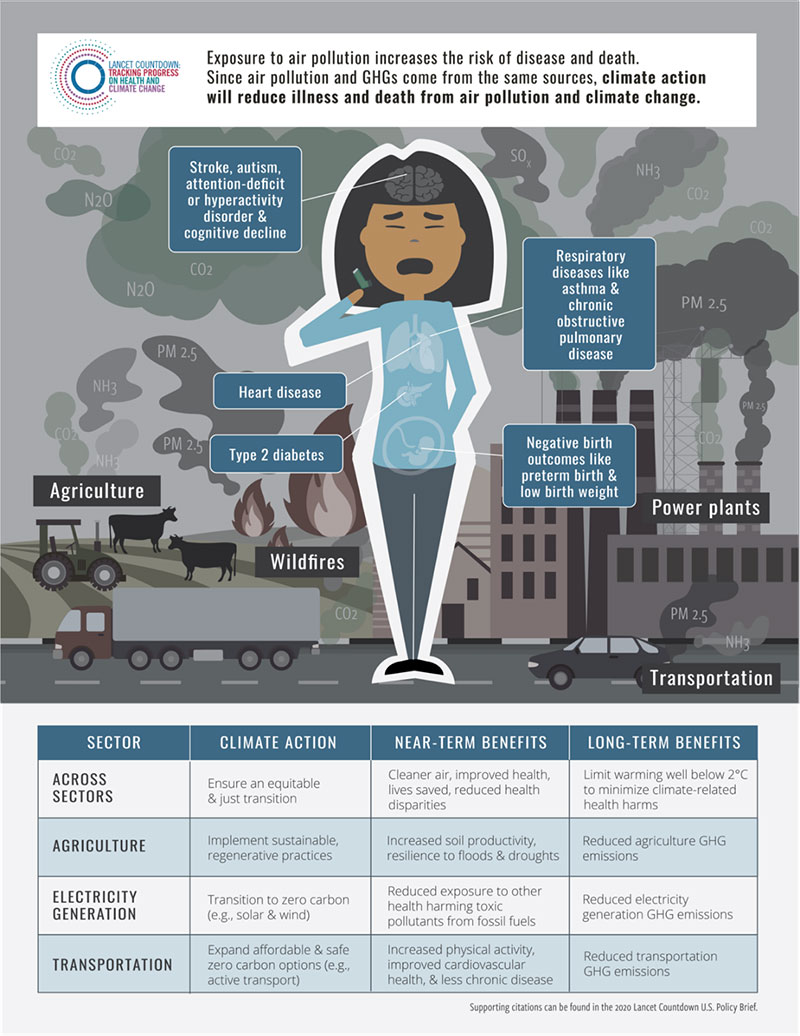
A transition to zero-carbon electricity generation will improve health and saves lives
The U.S. is making progress towards zero-carbon electricity generation: low-carbon sources of electricity generation rose to a record high 35%* in 2017, and renewable sources (excluding hydroelectric) rose to nearly 9%*._3 A transition to zero-carbon has been shown to be feasible by 2035, and a transition away from fossil fuels can save billions of dollars in health benefits alone._66, _67, _68 While everyone will benefit, this transition will especially protect vulnerable communities, and an equitable and just transition must ensure it is affordable for low-income communities.
Critical Insight:
Transitioning to zero-carbon energy in the U.S. will benefit public health today by improving the quality of our air, leading to longer and healthier lives across the country. It will also protect our health in the long-term by reducing the impacts of climate change. While these benefits will be felt across the country – reducing healthcare spending and sick days – a just and affordable transition to zero-carbon energy can particularly support better health in vulnerable and marginalized communities._3, _69, _70, _71, _72
Climate change and air pollution exacerbate inequalities in the U.S. that stem from systemic racism and other forms of discrimination. The impacts of air pollution in the U.S. are felt across the country, but particularly in Black and Latino communities._73 For example, rising pollution from the flaring of natural gas has been associated with up to a 50% higher chance of preterm births in mothers – who are largely Latina – living near oil and gas wells._74, _75, _76 Furthermore, tribes and Indigenous peoples are also often disproportionately impacted by air pollution and are particularly vulnerable to the impacts of climate change._77
Despite progress over the past few decades, different estimations find that air pollution from the use of fossil fuels still leads to between 50,000-100,000 early deaths each year in the U.S._41 This air pollution comes predominantly from the energy system, including power plants, transportation, and industry. Thus, phasing out the country’s remaining coal power plants and transitioning to zero-carbon transportation could save tens of thousands of lives across the U.S. each year._3 Research has shown that the health benefits of the energy transition can more than offset the costs of policies to reduce GHG emissions._78 Furthermore, engaging with communities that bear a disproportionate burden of these air pollution and climate change impacts can reduce existing equity gaps.
However the majority of electricity in the U.S. is still generated from fossil fuels, and in 2018 over 6,000 people* in the U.S. died prematurely from PM2.5 air pollution from power generation (Figure 2)._3 Coal power plants continue to cause almost 90%* of these deaths, even as the share of coal in national power generation is falling steadily, from 53% in 1990 to 28% in 2018*._3 Unfortunately, the decline in coal power generation in the U.S. is partly due to a shift towards natural gas, which still harms health and worsens climate change.
Critical Insight:
While natural gas can lower both GHG emissions and air pollution when it replaces coal power, it is not emissions-free. Power plants that use natural gas still produces around 42% the amount of carbon dioxide (CO2) as those that use coal per unit of electricity that is generated. F9 _79 Burning natural gas produces air pollution including nitrogen oxide (NOx), volatile organic compounds (VOCs), and particulate matter (PM), and can lead to ozone formation – all of which contribute to poor health, including respiratory illness._80, _81, _82, _83, _84
The use of natural gas in the U.S. rose by 35% over the past decade (Figure 4)._85, _86 In 2019, natural gas produced 35% of the total electricity generated in the U.S. compared to 18% in 2005._87 Over this same period, GHG emissions from natural gas power plants rose by 81%._88
Furthermore, the amount of natural gas that is vented and flared during production (i.e. at the well site) more than quadrupled from 2000-2018 in the U.S._35, _89 Several studies have found higher risk of asthma attacks and poor birth outcomes among communities living in proximity or downwind of oil and gas activity. _74, _75, _90, _91, _92, _93, _94, _95
Figure 4: Natural gas vented and flared in the U.S. between 2000-2018 (million cubic feet).
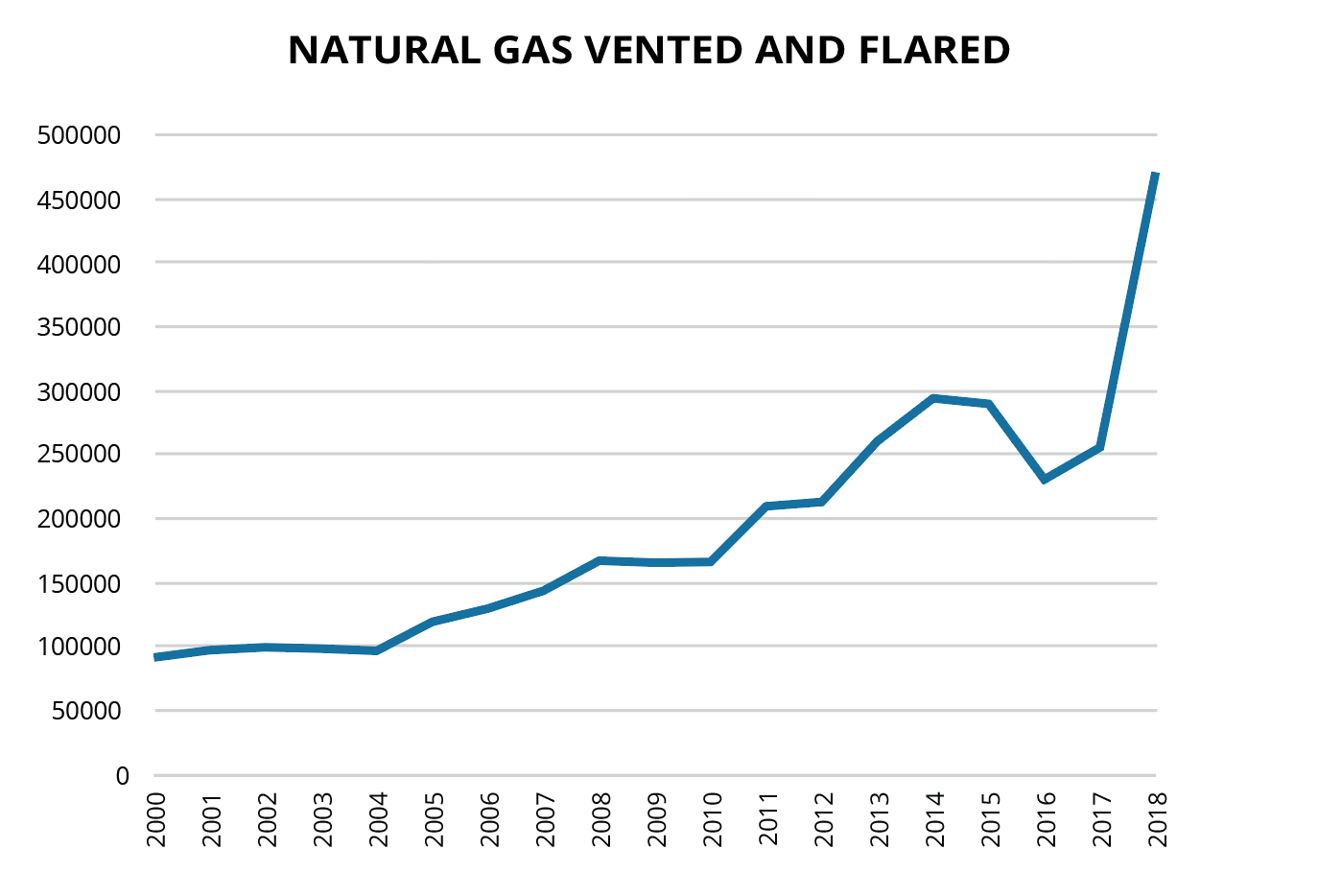
Source: Energy Information Administration. U.S. Natural Gas Vented and Flared (million cubic feet)._89 Additional note: 2017 datapoint is not currently available and so the trend from 2016 to 2018 was determined through linear interpolation.
The main component of natural gas is methane (CH4). Methane leaks occur throughout the entire natural gas supply chain. While transmission and storage of natural gas contributes to around 19% of this leaked methane (e.g., from leaky pipes), the majority (67%) of leaks occur during oil and gas production.96 The sector could cut methane emissions by approximately 70% using available emission-control technologies and operating practices, including leak detection and repair._97
Transport systems for clean air, low emissions, and physical activity
Active transport (e.g., walking and cycling) improves air quality, mitigates climate change, and increases physical activity levels, as endorsed by the American Heart Association’s policy statement._98 Yet, only about 3% of commutes in 2019 occurred via walking or cycling, with the majority occurring in vehicles._99
While the use of electricity for road transport increased by over 40 times* in the decade since 2007, just 0.06% of the energy used for road transport* in 2017 was electric._3 Thus, the vast majority of road transport energy came from fossil fuels, which, in addition to GHGs, contributed to over 12,000 premature deaths* in the U.S. in 2018 from transport-related PM2.5 (Figure 2)._3
An urgent transition to a zero-emission transportation system will lead to near-term health benefits and save 6,300 lives, prevent 93,000 asthma attacks, and generate $185 billion from health and climate benefits each year by 2050._100 In addition, affordable, more widely available zero-carbon public transit would promote physical activity as well as provide low-income households, youth, seniors, and persons with disabilities better access to resources.
Public health investments for climate-resilient communities
Public health spending is estimated to be between 1.5% and 3% of all U.S. health spending_101, _102, _103 and this lack of investment has dire consequences for health — whether in responding to the COVID-19 pandemic or ameliorating the impacts of climate change. In 2018-19, the U.S. spent nearly $13 per person* on climate change adaptation in the health sector_3, far less than what is needed to prevent the growing health impacts of climate change.
In order to respond to health threats, including those linked to climate change, funding priorities need to better reflect the fact that public health is critically important and is indeed essential for a productive workforce, healthy economy, and a thriving society. Climate change adaptation can occur through investments in resilient public health departments and programs that prevent adverse health impacts from occurring in the first place, such as climate disaster preparedness, surveillance, and early warning systems. Such investments are crucial to building resilient and equitable communities.
A healthy recovery from the COVID-19 pandemic
This year has been one of profound suffering and loss as the pandemic has taken a toll on both health and the economy. Yet, now is the time to take bold actions that address the connected health threats of climate change, the COVID-19 pandemic, and systemic racism. Climate change, health, equity, and economic objectives are not only mutually reinforcing but mutually dependent. The U.S. has an opportunity to re-imagine and invest in an equitable, just, and healthy future, featuring a clean energy economy with green jobs, protection for communities that are disproportionately affected, and strengthened resilience to future threats.
In March 2020, Congress passed the Coronavirus Aid, Relief and Economic Security Act (CARES Act), a $2.2 trillion economic stimulus bill — the largest in U.S. history — with the intent to protect American workers and small businesses from the economic fallout of COVID-19. Fossil fuel companies received billions from the CARES Act_104, on top of the yearly multi-billion dollar subsidies granted to the industry. Funds or subsidies to fossil fuel companies are bad investments from a health perspective and are unlikely to improve the market outlook for fossil fuel companies, especially as the price of renewable energy continues to drop._105
With thoughtful reforms, stimulus programs and redirected fossil fuel subsidies could represent an enormous opportunity to duly invest in the required actions for climate change discussed throughout this policy brief that will equitably improve health and well-being. These policies, which will define society for decades, need to be pursued urgently since our current and future health and pursuit of equity depend on it.
2020 U.S. Brief organizations and acknowledgements
U.S. Policy Brief Authors & Appendix Editors: Renee N. Salas, MD, MPH, MS; Paige Knappenberger Lester, MA; Jeremy J. Hess, MD, MPH
U.S. Policy Brief Critical Insight and Case Study Authors:
Critical Insight 1 – Climate Change and Vibrio: Caleb Dresser, MD and Caitlin Rublee, MD, MPH
Critical Insight 2 – Climate Action in Agriculture can Reduce Air Pollution and Minimize Climate Change: Eliyahu Y. Lehmann; Renee N. Salas, MD, MPH, MS; Paige Knappenberger Lester; Jeremy J. Hess, MD, MPH with critical input by (alphabetical) Erin Biehl, MSPH; Kritee Kritee, PhD; Lewis H. Ziska, PhD
Critical Insight 3 – Zero-Carbon Energy Will Improve the Quality of Our Air and Protect Vulnerable Communities: Melissa C. Lott, PhD
Critical Insight 4 – Natural Gas: Health and Climate Change Harms: Melissa C. Lott, PhD and Maria Castillo
Case Study – Compounding Crises of Our Time During Hurricane Laura Climate Change, COVID-19, and Environmental Injustice: Naomi Beyeler, MPH, MCP; Adrienne Hollis, PhD, JD; Juanita Constible, MSc; Allison Crimmins, MS, MPP; Lisa Patel MD, MESc, Jodi D. Sherman, MD
Case Study – The 2019 Floods in the Central U.S. Lessons for Improving Health, Health Equity, and Resiliency: Jesse E. Bell, PhD; Rachel Lookadoo, JD; Skye Wheeler, Christopher Dethlefs
Case Study – Promoting Food Security, Resilience and Equity during Climate-related Disasters: Cecilia Sorensen, MD; Hanna Linstadt, MD; Heidi Honegger Rogers, DNP, FNP-C; Erin Biehl, MSPH; Lewis H. Ziska, PhD
Case Study – Urban Green Space: Health Benefits and Reduction of Inequities: Paige Brochu, MS; Patrick Kinney, ScD, MS; Marcia P. Jimenez, PhD, MA, MSc; Peter James ScD, MHS; Kevin Lane PhD, MA
Additional Team Acknowledgements: Support, Logistics, & Review: Kelly Phouyaphone, MPH; Eliyahu Y. Lehmann. Infographic Designer: Mina Lee, MPA. Website, Figures/Tables, and Appendix PDF Design: D’lynne Plummer and team. Copy Editing: Kathryn Kempton Amaral, MS. Appendix Spanish Translation: Gabriela Haymes with the generous support of Human Rights Watch. Spanish Copy Editing: Felipe Benitez & Carmen M. Velez Vega, PhD, MSW
Review on Behalf of the Lancet Countdown (alphabetical): Jessica Beagley; MBBS; Marina Romanello, PhD; Nicholas Watts, MBBS
Review on Behalf of the American Public Health Association (alphabetical): Ivana Castellanos, MPH; Surili Sutaria Patel, MS; Katherine Robb, MSPH
Science and Technical Advisors (alphabetical): These science and technical advisors provided technical and review assistance but are not responsible for the content of the report, and this report does not represent the views of their respective federal institutions. John Balbus, MD, MPH; Allison Crimmins, MS, MPP
Combined Reviewer List for U.S. Brief & Appendix (alphabetical): Ploy Achakulwisut, PhD; Susan Anenberg, MS, PhD; Mona Arora, PhD, MSPH; Jesse E. Bell, PhD; Aaron Bernstein, MD, MPH; Naomi Beyeler, MPH, MCP; Erin Biehl, MSPH; Laura Bozzi, PhD; Robert Byron, MD, MPH; Juanita Constible, MSc; Cara Cook, MS, RN, AHN-BC; Tan Copsey, MA; Natasha DeJarnett, PhD, MPH; Michael A. Diefenbach, PhD; Robert Dubrow MD, PhD; Kristie Ebi, PhD, MPH; Matthew J. Eckelman, PhD; Sieren Ernst; Sarah Fackler, MA; Maryam Karimi, MPA, PhD, JD; Meghana Gadgil, MD, MPH, FACP; Ilyssa O. Gordon, MD, PhD; Chelsea L. Gridley-Smith, PhD; Adrienne Hollis, PhD, JD; Patrick Kinney, ScD, MS; Kritee Kritee, PhD; Yang Liu, PhD; Edward Maibach, PhD, MPH; Rachel Lookadoo, JD; Melissa C. Lott, PhD; Leyla Erk McCurdy, MPhil; Liz Mueller; Kari C. Nadeau, MD, PhD; Amruta Nori-Sarma, PhD, MPH; Jonathan Patz, MD, MPH; Rebecca Pass Philipsborn, MD, MPA; Stephen Posner, PhD; Rebecca Rehr, MPH; Heidi Honegger Rogers, DNP, FNP-C; Ananya Roy, ScD; Mona Sarfaty, MD, MPH; Emily Senay, MD, MPH; Jeffrey Shaman, PhD; Jodi D. Sherman, MD; Mark Shimamoto, MPH; Cecilia Sorensen, MD; Sarah Spengeman, PhD; Vishnu Laalitha Surapaneni, MBBS, MPH; Jon Utech, MBA, MPOD; Skye Wheeler; Jessica Wolff, MSN, MBA; Lewis H. Ziska, PhD
THE LANCET COUNTDOWN
The Lancet Countdown: Tracking Progress on Health and Climate Change is an international, multi-disciplinary collaboration that exists to monitor the links between public health and climate change. It brings together 38 academic institutions and UN agencies from every continent, drawing on the expertise of climate scientists, engineers, economists, political scientists, public health professionals, and doctors. Each year, the Lancet Countdown publishes an annual assessment of the state of climate change and human health, seeking to provide decision-makers with access to high-quality evidence-based policy guidance. For the full 2020 assessment, visit www.lancetcountdown.org/2020-report/.
THE AMERICAN PUBLIC HEALTH ASSOCIATION
The American Public Health Association (APHA) champions the health of all people and all communities. We strengthen the public health profession, promote best practices, and share the latest public health research and information. The APHA is the only organization that influences federal policy, has a nearly 150-year perspective, and brings together members from all fields of public health. In 2018, APHA also launched the Center for Climate, Health and Equity. With a long-standing commitment to climate as a health issue, APHA’s Center applies principles of health equity to help shape climate policy, engagement, and action to justly address the needs of all communities regardless of age, geography, race, income, gender and more. APHA is the leading voice on the connection between climate and public health. Learn more at www.apha.org/climate.
Recommended Citation: Lancet Countdown, 2020: 2020 Lancet Countdown on Health and Climate Change Policy Brief for the United States of America. Salas RN, Lester PK, Hess JJ. Lancet Countdown U.S. Policy Brief, London, United Kingdom.
Climate & Health in U.S. – Critical Insight 1: VibrioRecommendationsHealth Inequities & InjusticesAgricultural Interventions – Critical Insight 2: Agricultural ActionFossil Fuels, Air Pollution & Climate ChangeTransition to Zero-Carbon Electricity – Critical Insight 3: Energy & Equity – Critical Insight 4: Natural GasZero-carbon Transportation SystemsPublic Health InvestmentsHealthy Recovery from COVID-19Acknowledgements
CASE STUDY: Hurricane LauraCASE STUDY: 2019 FloodsCASE STUDY: Food Security CASE STUDY: Urban Green Space
